Overdose Prevention & Naloxone
- Dosing
- Identifying Opioid overdose
- Safe Use of Naloxone
Overdose is quite simply the medical condition involved with taking too much of a medication or drug. Because of the unregulated nature of a prohibition market, accurate dosing can be incredibly challenging as users may find that concentrations, cuts, potency and even substance make up are variable and unpredictable. Over the past number of years, we have witnessed a rise in “overdose” deaths, specifically caused by the introduction of Fentanyl and analogues into the supply of heroin, fake oxycontin and other opioids. Fentanyl is active in much smaller doses than other opioids and can make accurate dose prediction nearly impossible. While these “overdoses”, and resulting deaths, often involve someone who was intending to take an opioid taking more opioid than intended, the condition may be more accurately described as a poisoning, as the presence of Fentanyl or analogues was not known to the user or intended in the consumption. Some people are also speaking about the “overdose” deaths of the most recent Fentanyl epidemic as political killings, which speaks to the inaction of governments and law enforcement to prevent or address these poisonings because the people who are dying are often stigmatized as opioid users with intersectionally marginalized identities.
Being able to identify and respond to overdose are important skills for peers to have. When someone is experiencing an overdose, and specifically a depressant overdose, they will not be in a position to save their own life. When we are armed with the skills and knowledge to spot and address overdoses we can save someone else's life.
Potential Learning Outcomes
- Strategies for dose prediction.
- Identifying and addressing depressant overdose.
- Identifying and addressing stimulant overdose.
Discussion Topics
What is an overdose?
- When a person has so much drug in their bloodstream that the liver cannot detoxify (get rid of) the drug fast enough. Usually, the person experiences strong side effects or even death because too much drug in the bloodstream can stop your organs from getting oxygen
Public health messaging tells us to not use alone. What may prevent us from being able to follow this suggestion? How can we counter these challenges?
Opioid users identified many reasons why they are reluctant to use with others. These reasons include:
- Users didn’t want to share and diminish the hit
- Concern over theft of the gear or other personal belongings
- The stigma of asking a non-user to stay with them while using
- Wanting to hide use from friends or family
- Fear of police or being caught
Strategies to stay safe when using alone:
- Stay visible – Users stay out of sight to avoid getting busted. The ‘staying visible’ message is to encourage use in a place that is not completely isolated. It may be as simple as suggesting use in the lounge room instead of the bedroom.
- 50/50 (halve your hit) – Halving the hit is one way to lower the risk of overdosing when using alone. Some users may find they don’t need the 2nd half. Keep in mind, halving the dose will likely require more sterile equipment such as needles and syringes.
- Phone a friend first – A number of users said they always call a friend or talk to someone before they have a whack and while not necessarily saying they are doing, arrange for the friend to call them back fairly soon. This is a good strategy that others could try.
- check out resources below to access overdose prevention sites and remote overdose prevention supports
- Be aware and know your body – If you are alone and think you may have overdosed, call a trusted person or ambulance if you still can and unlock the door to wherever you are.
How do you try and stay safe when using alone?
This public health messaging pathologizes drug use and seeks to remove or reduce the enjoyable quality of it, which puts people at risk of overdosing because we are not talking about drugs in a sensible manner.
What is a test-dose? When should you use a test-dose? How does a test-dose inform dosing?
- Also called a taste-test, this is a process of taking not enough of a substance to get as high as you would like, but a small bit, to evaluate the potency. Since unregulated markets mean almost all of our drugs come with inconsistent potency and additives, this is an important thing to do with each new batch. Sometimes, one person will test the batch for a group; it is important to remember that individuals can also have wide variations in tolerance, body mass, metabolism and perception of potency.
How can you identify if someone has overdosed?
- It can happen fast before the needle is even out of the arm, or it can happen more slowly (minutes to hours)
- It might look like the person is sleeping
- Look/listen for:
- no breathing or very slow and difficult breathing
- dry mouth
- extremely small pupils
- bluish-coloured nails and lips
- very cold body
- confusion
- sleepiness/drowsiness
- muscle spasms
- vomiting
- seizures
- choking sounds
What does a stimulant overdose look like? Can naloxone help in a stimulant overdose?
- Naloxone will not work in a stimulant overdose, but use it if in doubt
- Stimulants: https://towardtheheart.com/stimulant-od-awareness
What are tips for reducing overdose?
- Always have a friend with you who knows what drugs you have taken and can help you in case of emergency
- If drinking or taking pills with heroin, do the heroin first. That way you can stay in better control of how high you are.
- Use drugs one at a time
- If you are mixing drugs, try to do less of each drug to avoid overdose
- Use less when you are sick
- If you are using after a period of abstinence, be careful and go slow
- Try using different methods from time to time (eg snort or swallow instead of injecting)
- You will enjoy your high more and your liver will thank you
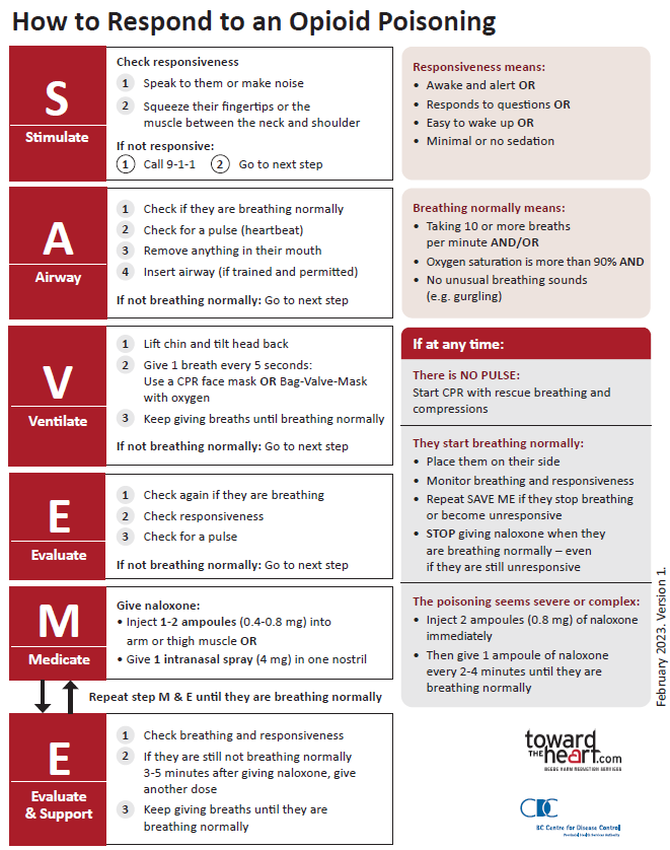
Responding to an Opioid Overdose using Naloxone and Rescue Breathing
Naloxone is an opioid antagonist that temporarily blocks the effect of opioids, used with rescue-breathing to reverse overdose. Available in 0.8mg intramuscular and 4mg nasal doses (availability varies), Naloxone is an essential emergency medication for people at risk of opioid overdose.
Carry Naloxone and know how to use it!
towardtheheart.com/naloxone-training
Call 911
Since 2017, the Good Samaritan Drug Overdose Act provides some legal protection for people who experience or witness an overdose and call 911 for help. The Act applies to anyone seeking emergency support during an overdose, including the person experiencing an overdose. The Act protects the person who seeks help, whether they stay or leave from the overdose scene before help arrives, as well as anyone else who is at the scene when help arrives.
For more information on what is and is not protected under the Good Samaritan Drug Overdose Act, check out this resource from Pivot Legal Society
https://www.pivotlegal.org/good_samaritan_drug_overdose_act_rights_card
When administering naloxone, the person who has overdosed will “revive” in a way that may trigger dope sickness. This can be worse when nasal naloxone is used. How can we support people after administering naloxone?
It is important to stay with someone who has overdosed after giving naloxone because:
- when the person wakes up they may have no memory of overdosing or receiving naloxone – explain to them what happened
- the person should be discouraged from using more opioids for at least 2 hours - remind them that withdrawal symptoms will start to wear off in half an hour, that using more opioids before the naloxone wears off will not help (because receptors are still blocked), and that using more will make it more likely for them to overdose again when naloxone does wear off
- to tell the emergency response team as much as you know (doses of naloxone given, timing, details of response)
If a person starts breathing on their own, but doesn't wake up, stop giving Naloxone, place them in the recovery position and monitor their breathing. See more on responding to overdose with prolonged sedation at towardtheheart.com/assets/uploads/1691694133K9B6FvAxwLjX1iIygf1X1dChEblLtkJZNgrakII.pdf
How can we ensure that we stay relatively safe and well while supporting or being supported through an overdose/revival?
What are user rooms, safer use facilities, OPS? What happens in such a facility and how does it keep users safer? How do sites like this come to be?
- https://www.nelsonstar.com/news/video-kootenays-first-overdose-prevention-site-opens-in-nelson/
- https://youtu.be/vZmIZzhC36g?si=JxmC4yYjC2_7SYq-
- https://www.cbc.ca/news/canada/british-columbia/smoking-substances-solutions-toxic-drug-crisis-1.6823856
- https://www.cbc.ca/news/canada/calgary/first-safe-inhalation-site-opens-lethbridge-1.4566743
Suggested Resources
Naloxone training resources:
towardtheheart.com/naloxone-training
Overdose prevention sites and services:
https://www.pivotlegal.org/scs_ops_map
https://towardtheheart.com/site-finder
https://lifeguarddh.com/ (Lifeguard App video: youtu.be/wyAfLzn1Z_g)
https://www.nors.ca/
https://www.brave.coop/
VCH Community overdose response video: youtu.be/C2X8bGa4wd8?si=N4oo4GOdakUiqRxC
Going Over Video: https://www.youtube.com/watch?v=mmHB1CZf-MU&list=PL40D8E249F1025C7E&index=4
Using Alone: a podcast: https://harmreduction.org/publication-type/podcast/eighty-nine/
Using Alone Module from AVI: https://docs.google.com/document/d/1ftUmFYmsMyrHguEpSleBWoiHXdLmdCgkRBIjiNkCBds/edit?usp=sharing
Remote Spotting - providing virtual peer witnessing support to prevent overdose:
https://ohrn.org/resources/remote-overdose-response-safety-plan/
https://ohrn.org/resources/how-to-remote-spot-someone-who-uses-drugs/
Recovery Position Module from AVI:
https://docs.google.com/document/d/1W3thgDjSIlvUYNTB-zEkjaIwgiQ5x57SYMX7oS4xE3k/edit?usp=sharing
Dilution harm reduction in the age of fentanyl
https://www.vice.com/en_us/article/wj3nmb/the-radical-new-fentanyl-trend-that-could-save-lives-and-screw-dealers
Responding to Opioid Poisoning with Prolonged Sedation: http://www.bccdc.ca/Documents/FINAL_Responding%20to%20Opioid%20Poisoning_Prolonged%20Sedation.pdf